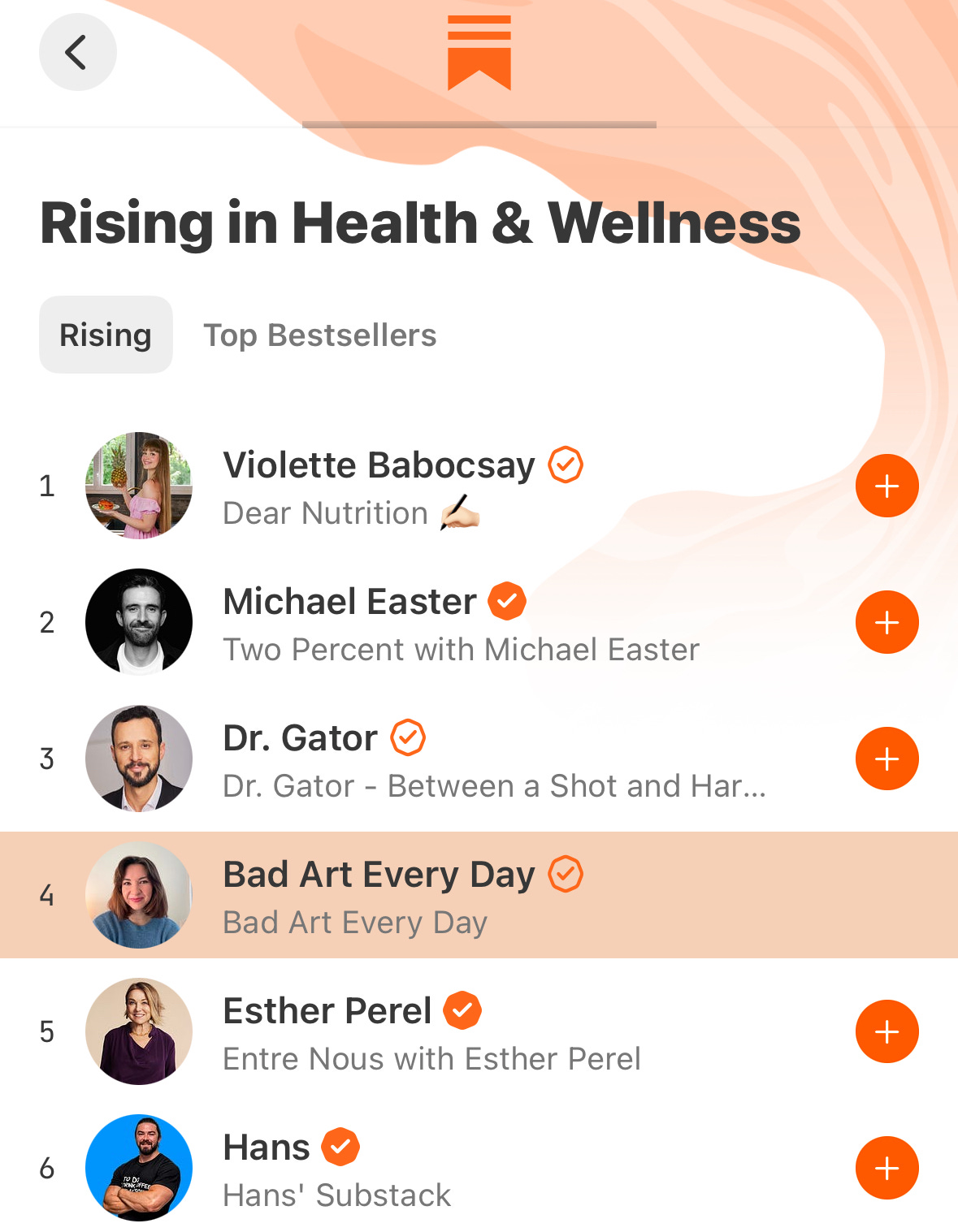
Why I'm Not Dr. Bad Art Every Day, MD
A small reflection on writing about lifestyle and wellbeing online without stating the fact immediately that I'm a physician, and why it's the right approach for me
As we move into winter, every year I think about what got me started in social media. A cold winter in Boston as an intern in a pediatrics rotation (aka 6am-6 pm) made me feel like I was learning a lot as a doctor, but losing the whimsical and creative parts of me that I didn’t have time for in that part of training. It was dark out whenever I was not in the hospital, and those shifts felt like 12 straight hours of the highest brain activity I could possibly put out. It was actually not unenjoyable, as I worked with new friends on a team and was treating adolescent and eating disorder patients. I was deeply engrossed, but I was aware of the playful part of me that I had always felt did not belong within the white coat.
For my own enjoyment, I knew I still needed to play and make good (or bad) art. I loved (and still love) Taylor Swift, am a romantic in all senses, and was on prom planning committee in high school. From all of this, you can get that I love a theme and love to love. I decided to start on TikTok by writing about living by the themes in the songs of Lover by Taylor Swift. Mostly, it was a challenge or devotion for me to keep thinking about things besides what I saw and learned in the hospital. It grew a few thousand followers in a month, which was huge traction for me at the time. TikTok has been mostly positive for me as a vehicle for creativity and expression, and I suspect it’s because my life has been busy and I love my clinical work. Since that time, I’ve grown my TikTok outside of the Taylor Swift niche mostly by continuing to post about lifestyle, habits, and pop culture themes I love.
When I began posting, I didn’t want my social media writing to be about medicine. I thought they needed to be separate anyway, and I was doing it to have access to the imaginative, VH1-loving, tumblr-having teen part of myself. At 26, I knew that I needed to hold that part of myself a little more tenderly and with a bit more celebration. I still thought it and medicine were separate.
Additionally, as stated, I WAS AN INTERN!
What did I know? Even at the time, I saw and knew of the misinformation around mental health online. I myself had fallen prey to some overpromising guides and coaches, and my early 20s library loan history was littered with self-help. As I still sometimes glibly say, it isn’t imposter syndrome if you truly are not yet skilled at something (which was developmentally normal for an intern!). I did not feel equipped to speak to a non-specific audience about psychiatry. Even as a board-certified adult psychiatrist now, I tend to lean away from generalizations or specific advice. Navigating mental health is like navigating giving someone directions to a place: the same advice that would get one person closer to where THEY want to be could bring another person in the totally wrong direction. If I send out information to a broad general public in the form of even longer social media posts, the algorithm doesn’t show it to people who it is the most accurate for. Algorithms direct what you see based on what is most salient—and salience can be an anxiety compulsion, a trigger of trauma, a video or idea coherent with the negative evaluation that depression causes in one’s cognitions. I felt MUCH more confident to talk about Taylor Swift albums, and eventually, confident in talking about small ways to try to be more creative, organized, and present like the good books and magazines I had once read as a teen (not the self-help book era though).
Quite a bit has changed in the last year, and overall that change has been quite positive.
I completed my fourth year of adult psychiatry residency and won a resident teaching award for creating a more robust curriculum for weekly psychotherapy lectures. I was recruited to start a podcast with my friend and fellow psychiatry trainee, Presro, and we’ve completed two seasons for a total of 40 episodes thus far, and even got asked to speak at the American Psychiatry Association for a panel on social media and psychiatry. This past month, I found out I passed my adult psychiatry boards, meaning I am now a board-certified psychiatrist (!!!) after 8 years of medical training. I also started child fellowship, which I’ve found challenging and enlivening. Finally (this is an annoying list now I’m sorry), I became dedicated to cultivating this space for longer writing here on Substack, and for finding a way to see if the time I put into this writing can be paid or sustainable, so that when I do finish training and continue on in life, I won’t need to be always behind on something or rushing.
With these milestones and with the years of training, last year I felt comfortable enough to say yes to the podcast opportunity when it was presented. Part of my hopes in healthcare and interest is in systems of care and education, and like anyone who cares about an ideal in a big, sometimes overly complex hierarchy, I like to complain about what should be different and how I would do it. When Preston was recruited by Dr. Glaucomflecken to do a podcast, I remember telling him how awesome that opportunity was, and how exciting both the education and conversations he would have would be. When he then surprised me by asking me (?!! was my internal reaction), it was a bit of a…well, excuse my language but a, “shit or get off the pot” situation. If you want a system to change, if you do feel prepared enough (I did at that point), and the opportunity presents, you need to take it or you need to chill a little on your complaining. So I said yes, and the first ten episodes functioned as a bit of exposure therapy for me (and Preston, for whom the podcast format was also new).
Over the year of creating longform, nuanced, and highly caveat-ed content around mental health on the podcast and women’s health information on here, the anxiety has lowered. Being a full on attending level, board-certified psychiatrist also helps. Finally, the amount of misinformation in the last year alone from the administration on everything from vaccines to SSRI’s to how mental health treatment works has been a propeller for me to research, write as well as possible, and get in the arena. I see the pregnant patients in my clinic who are struggling and then this misinformation makes them feel like getting care (which is shown to help them AND fetal development and longterm child outcomes) is a failing. I see the fear people have about what the world makes of their child with autism. I am prepared enough—we need voices out there with experience and without a supplement line.
This leads us to the question—why I am still not Bad Art MD on socials.
When I was younger, seeing that someone was a therapist or a doctor made me assume they were like my father, who is a retired primary care doctor from a small midwestern farm town. He does good things like he’d never thought to do anything else, and I strive to be like him. Growing up and being in the world, I learned that not every person is like him—whether that person is another doctor, a nurse, a businessman, a teacher, an influencer. I still want to be like him, but between self-help content online and realizing the amount of negative experiences people have in healthcare, I haven’t always wanted people to feel the information or things I write about are from a physician. I wanted them to see if they liked it on their own, without having too much influence on them. I believe that the public does need to seek better information, and re-orient to people who dedicate their lives to understanding something—teacher, caregivers, researchers, doctors. However, I know that when someone says, “I’m a doctor, trust me…” to a crowd of people, the immediate trust and belief is still a part of the privilege of being in the field, even online. When I speak to my patients, cite research, or on the podcast do an overview on standard of care, I want people to trust that over “trust me bro” influencers. When I talk about ideas to help you be a little more mindful, a little more present, and to address your anxiety differently, I want it to have the feeling of two friends over coffee. I want you, as my reader, to feel we are two peers sitting down and considering something, and that you are the expert of your experience and what suggestions might feel good. Ultimately, with my patients I want this collaborative, longitudinal clinical relationship, too. In public, collaboration and mutual influence cannot happen when speaking to a contextless, social media crowd, and especially not in 1 minute or a paragraph.
I believe many people out there who identify by their credentials are doing absolutely crucial work, work that is more needed than ever. I am glad that I’ve stepped a bit more into acknowledging on here and the podcast my daily life and expertise in psychiatry, especially in working in eating disorders, with chronic pain, and in pregnancy. As for my daily writing, I hope it comes to you like a comfort, a friend, or a good idea, and gives you 0% white coat anxiety. At present, this is the way that I do my part to impact the health information that we all swim in online every day.
Thank you for being a part of this, and supporting my writing over the years. This community and writing for you has made me understand that creativity and care for patients can go hand-in-hand.
Take care and take your time,
Margaret of Bad Art Every Day



As someone who does have ‘white coat fever’ your considered, nuanced approach is exactly why I subscribed. ❤️